Diabetes type 1 hesi case study – Prepare to delve into the intricacies of diabetes type 1 with our HESI case study. Join us as we unravel the complexities of this condition, from its enigmatic origins to its multifaceted management strategies. Along this captivating journey, we’ll unravel the mysteries of insulin deficiency, explore the delicate balance of blood glucose regulation, and uncover the profound impact of lifestyle choices on this lifelong companion.
Diabetes type 1, a formidable adversary in the realm of chronic diseases, demands a nuanced understanding. We’ll dissect its pathophysiology, unraveling the intricate interplay between the pancreas, immune system, and insulin. Together, we’ll navigate the diagnostic labyrinth, deciphering the intricacies of blood glucose testing and antibody screening.
Our quest will culminate in a comprehensive exploration of insulin therapy, empowering you with knowledge about types, administration methods, and monitoring techniques.
Definition and Overview of Diabetes Type 1
Type 1 diabetes, also known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition where the pancreas produces little to no insulin.
Insulin is a hormone that helps glucose, or sugar, enter cells for energy. Without insulin, glucose builds up in the bloodstream, leading to various health complications.
Causes of Type 1 Diabetes
- Autoimmune response:The body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas.
- Genetic factors:Certain genetic variations increase the risk of developing Type 1 diabetes.
- Environmental triggers:Viral infections, dietary factors, and stress may play a role in triggering the onset of the condition.
Symptoms of Type 1 Diabetes
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Increased hunger
- Fatigue
- Blurred vision
Prevalence of Type 1 Diabetes
Type 1 diabetes affects approximately 5-10% of all diabetes cases. It typically develops in children and young adults but can occur at any age.
Difference between Type 1 and Type 2 Diabetes
Unlike Type 1 diabetes, Type 2 diabetes is characterized by insulin resistance, where the body does not respond properly to insulin. Type 2 diabetes is more common and often develops in adulthood, while Type 1 diabetes requires lifelong insulin therapy.
Pathophysiology of Diabetes Type 1
Type 1 diabetes is an autoimmune disease characterized by the destruction of insulin-producing beta cells in the pancreas. Insulin is a hormone that regulates blood glucose levels, and its deficiency leads to hyperglycemia, or high blood sugar.
Role of the Pancreas in Insulin Production and Regulation
The pancreas is a gland located behind the stomach that plays a crucial role in digestion and hormone production. The pancreas contains clusters of cells called islets of Langerhans, which are responsible for producing and releasing insulin and glucagon.
Insulin is released into the bloodstream when blood glucose levels rise after a meal. Insulin binds to receptors on cells throughout the body, allowing glucose to enter the cells and be used for energy or stored for later use.
Immune System Attack on Beta Cells
In Type 1 diabetes, the immune system mistakenly attacks and destroys the beta cells in the pancreas. This process is mediated by T-cells, which are white blood cells that normally protect the body from infection.
The exact cause of this autoimmune attack is unknown, but it is thought to involve a combination of genetic and environmental factors. Certain genetic markers have been linked to an increased risk of developing Type 1 diabetes, and exposure to certain viruses or other environmental triggers may also play a role.
Consequences of Insulin Deficiency
The destruction of beta cells leads to a deficiency of insulin, which has several consequences:
- Hyperglycemia:Without insulin, glucose cannot enter cells and blood glucose levels rise.
- Ketoacidosis:In severe insulin deficiency, the body begins to break down fat for energy, producing ketones as a byproduct. Ketones can accumulate in the blood and cause a life-threatening condition called ketoacidosis.
Hyperglycemia and ketoacidosis can lead to a variety of symptoms, including thirst, frequent urination, fatigue, blurred vision, and nausea. If left untreated, these complications can be fatal.
Diagnosis and Management of Diabetes Type 1
Diagnosing and managing diabetes type 1 involves several key steps, including blood glucose testing, antibody screening, and implementing an effective treatment plan that focuses on insulin therapy, lifestyle modifications, and regular monitoring.
Diagnostic Criteria
The diagnosis of diabetes type 1 relies on specific criteria, including:
- Fasting blood glucose level: A fasting blood glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions.
- Random blood glucose level: A random blood glucose level of 200 mg/dL (11.1 mmol/L) or higher, accompanied by classic symptoms of diabetes, such as excessive thirst, frequent urination, and unexplained weight loss.
- Oral glucose tolerance test (OGTT): An OGTT involves measuring blood glucose levels after consuming a sugary drink. A blood glucose level of 200 mg/dL (11.1 mmol/L) or higher two hours after the drink indicates diabetes.
In addition to blood glucose testing, antibody screening is often performed to detect the presence of autoantibodies, such as islet cell antibodies (ICAs) and glutamic acid decarboxylase antibodies (GADs), which are associated with diabetes type 1.
Insulin Therapy
Insulin therapy is the cornerstone of diabetes type 1 management. It involves administering insulin to replace the body’s inability to produce its own insulin.
There are several types of insulin available, each with different durations of action:
- Rapid-acting insulin: Starts working within 15 minutes and lasts for 3-4 hours.
- Short-acting insulin: Starts working within 30 minutes and lasts for 6-8 hours.
- Intermediate-acting insulin: Starts working within 1-2 hours and lasts for 12-18 hours.
- Long-acting insulin: Starts working within 1-2 hours and lasts for 24 hours or more.
Insulin can be administered using various methods, including:
- Injection: Insulin can be injected subcutaneously (under the skin) using a syringe or an insulin pen.
- Insulin pump: An insulin pump is a small, computerized device that delivers insulin continuously through a small tube inserted under the skin.
Regular monitoring of blood glucose levels is essential to adjust insulin doses and ensure optimal control.
Lifestyle Management
Lifestyle management plays a crucial role in managing diabetes type 1. This includes:
- Diet: Following a healthy diet that is low in carbohydrates and high in fiber can help control blood glucose levels.
- Exercise: Regular physical activity helps improve insulin sensitivity and lower blood glucose levels.
- Blood glucose monitoring: Regular blood glucose monitoring is essential for managing diabetes effectively and preventing complications.
Complications of Diabetes Type 1: Diabetes Type 1 Hesi Case Study
Complications of diabetes type 1 can be both acute and long-term. Understanding these complications and their management is crucial for individuals with diabetes type 1 to maintain their overall health and well-being.
Acute Complications
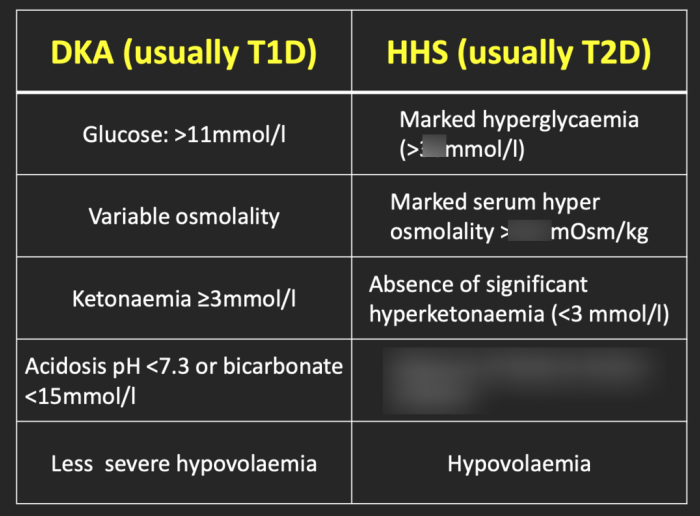
Acute complications of diabetes type 1 include hypoglycemia and diabetic ketoacidosis (DKA).
After reviewing the diabetes type 1 HESI case study, I found myself pondering the complexities of chemical reactions. This led me to explore the net ionic equation for the reaction between manganese (II) and tin(IV) chloride . Understanding the intricacies of these reactions helps us appreciate the delicate balance of our bodies and the importance of maintaining proper blood sugar levels in diabetes type 1.
- Hypoglycemia:Occurs when blood glucose levels drop too low, typically below 70 mg/dL. Symptoms include sweating, shakiness, hunger, irritability, and confusion. Severe hypoglycemia can lead to seizures, coma, and even death if not treated promptly.
- Diabetic ketoacidosis (DKA):A serious and life-threatening condition that develops when the body cannot use glucose for energy and breaks down fat instead. This produces ketones, which can lead to dehydration, electrolyte imbalances, and coma. Symptoms include thirst, frequent urination, nausea, vomiting, and abdominal pain.
Long-Term Complications, Diabetes type 1 hesi case study
Long-term complications of diabetes type 1 can affect various organs and systems in the body.
- Cardiovascular disease:Diabetes type 1 increases the risk of heart disease, stroke, and peripheral artery disease. High blood glucose levels can damage the blood vessels and lead to plaque buildup, narrowing the arteries and reducing blood flow.
- Retinopathy:Damage to the blood vessels in the retina can lead to diabetic retinopathy, a leading cause of blindness in people with diabetes. Symptoms include blurred vision, floaters, and vision loss.
- Nephropathy:Diabetes type 1 can also affect the kidneys, leading to diabetic nephropathy. This can cause proteinuria (protein in the urine), high blood pressure, and eventually kidney failure.
- Neuropathy:Damage to the nerves can cause diabetic neuropathy, which can affect sensation, motor function, and autonomic functions. Symptoms include numbness, tingling, pain, and weakness.
Importance of Regular Monitoring and Screening
Regular monitoring of blood glucose levels and screening for complications is essential for individuals with diabetes type 1. This allows for early detection and intervention, which can help prevent or manage complications and maintain overall health.
- Blood glucose monitoring:Frequent blood glucose monitoring helps ensure blood glucose levels stay within target ranges and allows for timely adjustments in insulin dosage.
- Screening for complications:Regular eye exams, kidney function tests, and nerve function assessments can help detect early signs of complications and allow for appropriate treatment.
Nursing Care for Patients with Diabetes Type 1
Nurses play a crucial role in the care of patients with diabetes type 1. They provide education, support, and guidance to help patients manage their condition effectively.
Principles of Patient Education and Support
Nurses provide patient education on various aspects of diabetes management, including:
- Insulin administration techniques
- Blood glucose monitoring
- Healthy eating and lifestyle choices
- Preventing and managing complications
Support is essential for patients with diabetes. Nurses provide emotional support, encourage self-management, and help patients navigate the challenges of living with a chronic condition.
Importance of Interdisciplinary Collaboration in Diabetes Management
Diabetes management requires a team approach involving various healthcare professionals. Nurses collaborate with physicians, dietitians, pharmacists, and other specialists to provide comprehensive care. This collaboration ensures that patients receive the best possible care and support from all disciplines involved in their management.
FAQ Summary
What is the primary cause of diabetes type 1?
Diabetes type 1 is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the beta cells in the pancreas, which are responsible for producing insulin.
How does diabetes type 1 differ from diabetes type 2?
Diabetes type 1 is an autoimmune condition that typically develops in childhood or adolescence, while diabetes type 2 is a metabolic disorder that usually develops in adulthood and is associated with insulin resistance and impaired insulin secretion.
What are the key symptoms of diabetes type 1?
Common symptoms include excessive thirst, frequent urination, unexplained weight loss, increased hunger, fatigue, and blurred vision.
How is diabetes type 1 managed?
Management involves lifelong insulin therapy, regular blood glucose monitoring, a balanced diet, regular exercise, and lifestyle modifications.